Herpes simplex virus type 1 (HSV-1) is widely recognized for its role in cold sores and facial lesions; however, its influence extends into the realm of neurological health. Emerging evidence now indicates that HSV-1 can infiltrate the brain and central nervous system, leading to significant neuropathological consequences. A recent study spearheaded by experts from the University of Colorado and the University of Bourgogne in France offers critical insights into the viral pathways and neurological implications associated with HSV-1 infections. Understanding how this virus not only survives but also propagates within various brain regions is crucial for mitigating potential long-term health risks.
Traditionally, HSV-1 invades the central nervous system via the trigeminal or olfactory pathways. While these entry points are relatively understood, the mechanisms through which HSV-1 proliferates within the brain are still shrouded in uncertainty. Neurologist Christy Niemeyer emphasizes the necessity of charting these paths to elucidate how HSV-1 might underlie cognitive decline and neurodegenerative disorders, including Alzheimer’s disease.
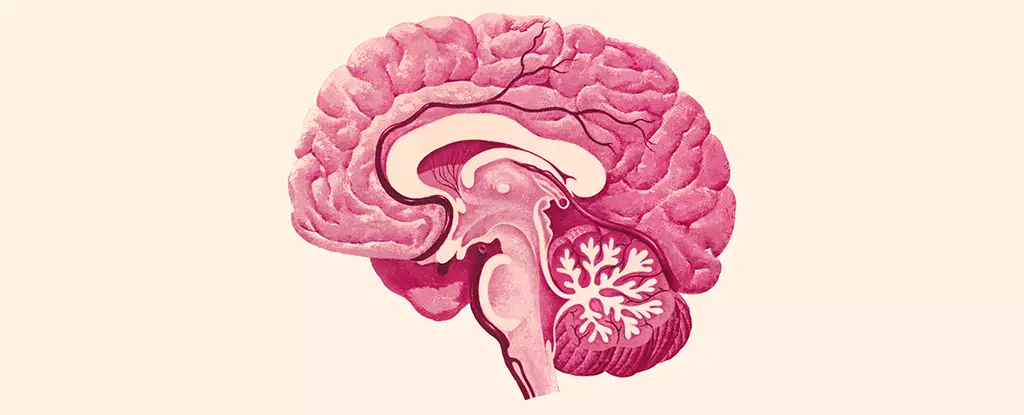
The recent research meticulously documented the brain regions susceptible to HSV-1 infection, identifying critical structures such as the brain stem and hypothalamus as battlegrounds for the virus. The brain stem regulates essential life functions such as cardiac and respiratory rhythms, while the hypothalamus governs mood, appetite, and hormonal balance. The potential disruption of these vital areas gives rise to questions about the broader implications of HSV-1 presence in the brain.
Conversely, some regions, including the hippocampus—central to memory processing—and the cortex—which contributes to executive functions like attention—did not exhibit HSV-1 antigens. This intriguing finding underscores the selective nature of viral effects on different brain regions and emphasizes the necessity for further investigation into the clinical outcomes associated with this selective neuronal involvement.
The immune response in the central nervous system is orchestrated by microglia, which act as the brain’s resident immune cells. This research highlighted how microglial activation is concomitant with HSV-1 infection, leading to an inflammatory response. Remarkably, inflammation persisted in certain brain regions even after the virus was no longer detectable. This prolonged state of inflammation raises concerns about chronic neurological damage, hinting at a potential vicious cycle where ongoing immune activation could exacerbate neuronal injury.
Niemeyer notes that even in the absence of full-blown encephalitis—an acute and severe inflammation of the brain—HSV-1 can disrupt normal brain functioning. This disruption is indicative of the broader implications for long-term cognitive health, particularly as chronic inflammation is increasingly recognized as a contributing factor to neurological disorders.
The intricate relationship between HSV-1 infections and neurodegenerative diseases is not new; the relevance of viral infections in the etiology of diseases like Alzheimer’s has garnered much attention in scientific circles. The ongoing inflammation instigated by HSV-1 might serve as a catalyst for neurodegenerative processes, particularly in vulnerable populations. The study suggests that regions concurrently affected by HSV-1 and shown to deteriorate in Alzheimer’s patients may represent critical areas for therapeutically targeted research.
Furthermore, the persistence of inflammatory responses in microglia could contribute to neuroinflammation, a hallmark of many neurological diseases. Niemeyer asserts that this chronic inflammatory state may trigger or accelerate various neurodegenerative disorders, necessitating a deeper investigation into the mechanisms linking HSV-1 to detrimental cognitive outcomes.
As researchers continue to explore the interplay between viral infections and brain health, the findings from this study on HSV-1 provide a vital groundwork for understanding the complexities of neurodegenerative diseases. By mapping the viral invasion routes and assessing the resulting inflammation, scientists can not only bolster their grasp of HSV-1’s implications for neurological disorders but also pave the way for potential interventions. This research represents a critical step forward in uncovering the hidden connections between common viral infections and devastating diseases like Alzheimer’s, ultimately illuminating pathways for therapeutic innovations.