The emergence of a critical case of avian influenza in Louisiana has catalyzed anxiety regarding the potential for a bird flu pandemic. This incident, noted as the first severe human case of the H5N1 strain in the United States for 2024, has raised alarms within public health agencies. The patient, an elderly individual with pre-existing health conditions, is hospitalized in critical condition, marking a significant escalation in the context of a virus that has otherwise remained somewhat contained in human populations. As the United States grapples with an uptick in avian influenza cases, this latest incident signifies a pivotal moment in understanding the risks and realities associated with zoonotic diseases.
Indicators of a Potential Pandemic
The gravity of this situation is underscored by the statistics: a total of 61 avian influenza cases have been documented in the U.S. during the ongoing outbreak. Most infected patients previously reported mild symptoms and were able to recover at home; however, this critical case serves as a sobering reminder of the virus’s potential lethality. Health experts note that avian influenza, particularly the H5N1 strain, has claimed lives in up to 50% of documented cases in other countries over the past two decades, reinforcing the need for vigilance. The recent case also resonates with similar instances abroad, such as the severe case reported in a Canadian teenager, framing a pattern that could threaten public health on a larger scale.
Understanding the Transmission Dynamics
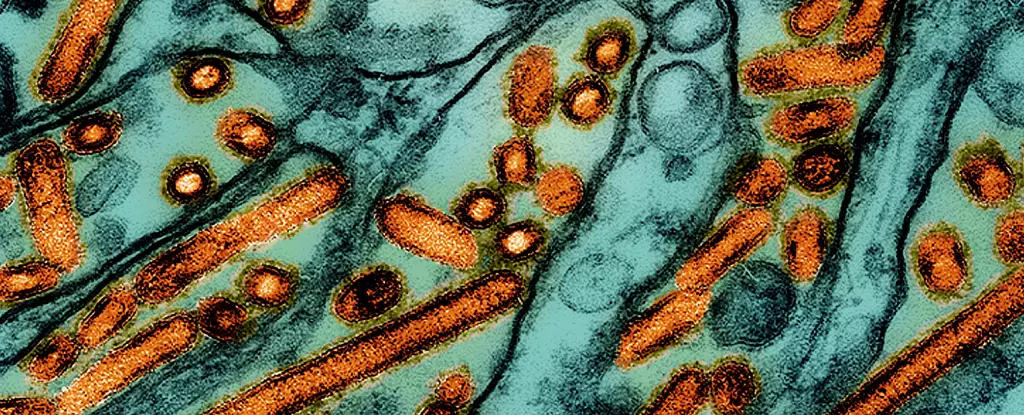
According to the Centers for Disease Control and Prevention (CDC), the Louisiana patient was exposed to sick or deceased birds in backyard flocks, highlighting the critical role of animal contact in the transmission of avian influenza to humans. Genetic analysis of the virus indicated it belonged to the D1.1 genotype, a strain that has been increasingly detected in both wildlife and poultry across North America. This genetic variant varies significantly from the B3.13 strain, which has been associated with milder symptoms in humans, raising questions about the virulence and transmission potential of D1.1.
Moreover, the lack of robust surveillance for avian influenza infections in animal populations may mask the true extent of exposure risks to humans. The CDC has acknowledged cases in which people contracted the virus with no identifiable contact with infected birds—a notion that underlines the uncertainty surrounding asymptomatic human-to-human transmission. If indeed such transmission is occurring, the implications for public health are profound and necessitate a reevaluation of monitoring efforts.
In response to this growing concern, California has declared a state of emergency, empowering governmental agencies to swiftly mobilize resources and enhance surveillance. Governor Gavin Newsom’s administration is determined to bolster the state’s monitoring framework and support the agricultural sector amid rising fears of further outbreaks. This proactive approach reflects a broader understanding that rapid responses will be crucial in averting the scenario of widespread transmission.
Federal authorities are also preparing for potential human cases by stockpiling vaccines against bird flu. This preparation is indicative of a serious commitment to mitigating the possible consequences of an avian influenza pandemic. Recent studies have unveiled promising data from experimental mRNA vaccines, showcasing their efficacy in protecting laboratory animals from the virus—an encouraging development in the realm of infectious disease management.
The urgency for enhanced surveillance is echoed by experts like Rebecca Christofferson from Louisiana State University, who emphasizes the possibility that unnoticed cases of animal-to-human virus spillover may be occurring undetected. Amid ongoing concerns, skepticism remains among researchers regarding the adequacy of current monitoring systems. Epidemiologist Meg Schaeffer asserts that various factors indicate that avian influenza is on the cusp of spreading more widely, thus heightening the need for immediate, tactical responses.
As the U.S. Department of Agriculture takes steps to require that raw milk samples from dairy farms be reported if found to contain the virus, the situation underscores a critical intersection between veterinary public health and food safety. The potential for raw milk to act as a transmission vector adds yet another layer of complexity in managing zoonotic diseases, requiring comprehensive strategies that address both animal health and human food consumption patterns.
The Louisiana avian influenza case juxtaposes the world’s experience with past pandemics against present hazards, surfacing profound questions regarding preparedness and response mechanisms. As both public health officials and the populace at large navigate this unfolding scenario, the call to remain vigilant is paramount. The lessons learned from this situation will be crucial not only for managing avian influenza but also for any similar public health threats in the future. Sustaining awareness, conducting ongoing research, and enhancing surveillance are essential actions that will determine the trajectory of this evolving health crisis.