In the realm of public health, few issues reveal the depth of systemic discontent and political brinkmanship quite like the ongoing NHS staffing disputes. For months, the illusion persisted that all stakeholders aligned toward a common goal: a stronger, more resilient NHS. However, beneath the surface, cracks widen, exposing divergent interests and unbridgeable mistrust. The recent negotiations between the health secretary and the BMA offer a stark reminder that appearances of cooperation often mask underlying fractures. As a critic of superficial narratives, I see these conflicts not as isolated disputes but as symptomatic of a system desperately clinging to hope while teetering on the edge of peorization.
The Myth of Goodwill and the Reality of Injustice
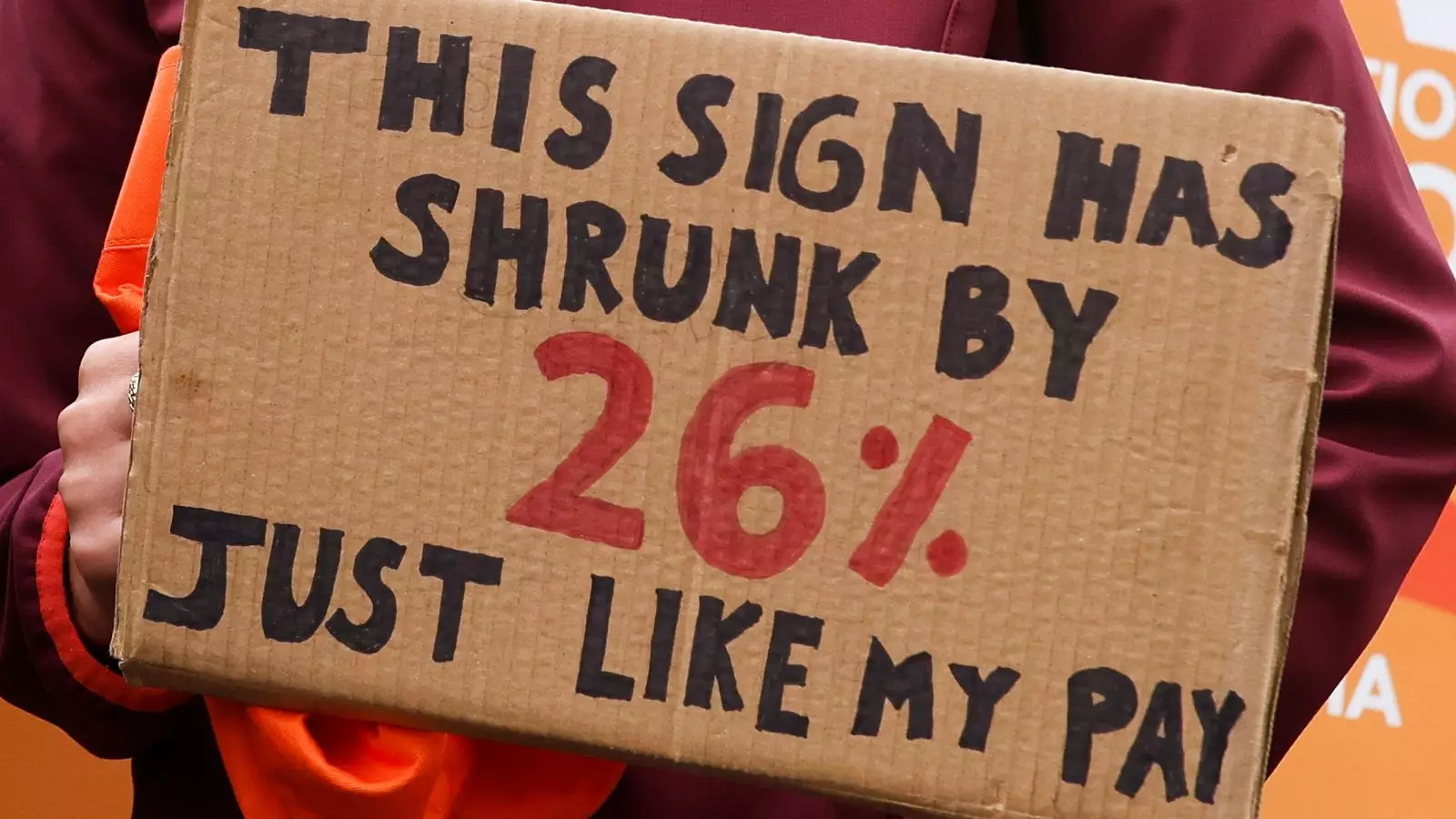
The government pitches its NHS reform as forward-looking and ambitious, promising a decade of transformation rooted in innovation and efficiency. Yet, this vision is fundamentally undermined by its failure to address the core issue: fair compensation for medical professionals who have been undervalued for nearly two decades. The BMA’s demand for a 26% pay restore is not an unreasonable upheaval; it’s a desperate cry from exhausted doctors who have endured stagnation in their wages while their workload and stress levels skyrocketed. The government’s claim of a 29% pay rise over recent years appears more hollow than helpful—highlighting a crucial disconnect: who truly benefits, and at what cost? When policymakers prioritize rhetoric over justice, public trust erodes and the delicate fabric holding the NHS together frays further.
The Power Struggle Over Public Perception
The language surrounding the strikes has devolved into a blame game, with neither side willing to accept responsibility without weaponizing it. Politicians like Wes Streeting frame their efforts as safeguards, emphasizing local decision-making to minimize harm, while unions argue that such measures compromise patient safety. The truth is more complex. The NHS’s systemic staffing shortages and chronic underfunding create fertile ground for chaos. The government’s insistence on a ‘trust-led’ approach seems more like abdication of responsibility than strategic ingenuity. Meanwhile, public opinion has shifted, less sympathetic to union frustrations and more critical of any disruption—an indication of how effectively political narratives can manipulate public sentiments, often at the expense of the very staff who keep the system afloat.
The Underlying Crisis of Underpayment and Exhaustion
The heart of the discord lies in recognition—or the glaring lack thereof. For years, resident doctors and junior staff have been invisible in political discussions, their labor undervalued, their sacrifices dismissed. The claim of an 18-pound-an-hour wage starkly reflects the economic invisibility of frontline healthcare workers. It’s not just about pay; it’s about dignity and respect. When the state neglects to adequately compensate those who save lives daily, it sends a powerful message about priorities. The ensuing strikes are, therefore, a symptom of a deeper moral failure—a failure to value human labor that is critical to societal well-being.
The Clash of Visions: Local Autonomy vs. Central Control
Wes Streeting’s proposals for localized decision-making may seem pragmatic on paper, but they threaten to deepen fragmentation rather than mend it. Relying on trust leaders to decide on urgent care creates a patchwork of standards, risking inconsistent patient safety measures. Strikes disrupting non-critical services reveal an underbelly of systemic vulnerability: amateurish improvisations that mask the fundamental crisis—an NHS that is increasingly unable to promise equitable, safe care under current resource constraints. For many, this approach suggests a government that prefers decentralization not as a devolution of responsibility but as a convenient way to dodge accountability.
The Deepening Divide and the Future of the NHS**
Ultimately, the NHS is caught in a crisis of credibility, resources, and morale. The strike disputes reveal a broader challenge facing the liberal center: how to balance fiscal responsibility with genuine investment in people who are the backbone of public health. Disharmony among healthcare providers and government officials is not merely a bureaucratic issue; it’s emblematic of a system under siege, often run on goodwill and fragile consensus rather than sustainable funding. Without decisive action that genuinely restores fairness and respects frontline workers, the path forward remains littered with the dangers of further unrest, loss of trust, and eventual systemic collapse. The question is not how to patch superficial fixes but whether policymakers are willing to confront the uncomfortable truths about the NHS’s fundamental deformities.